Gangrenous kidney, also known as renal or kidney infarction, is a rare condition that occurs when blood flow to the kidney is blocked or reduced, leading to tissue death (necrosis) and potentially irreversible damage.
The most common cause of renal infarction is a blood clot, which may originate from the heart, a blood vessel in the kidney, or another part of the body. Other causes include arterial embolism, atherosclerosis, vasculitis, and trauma.
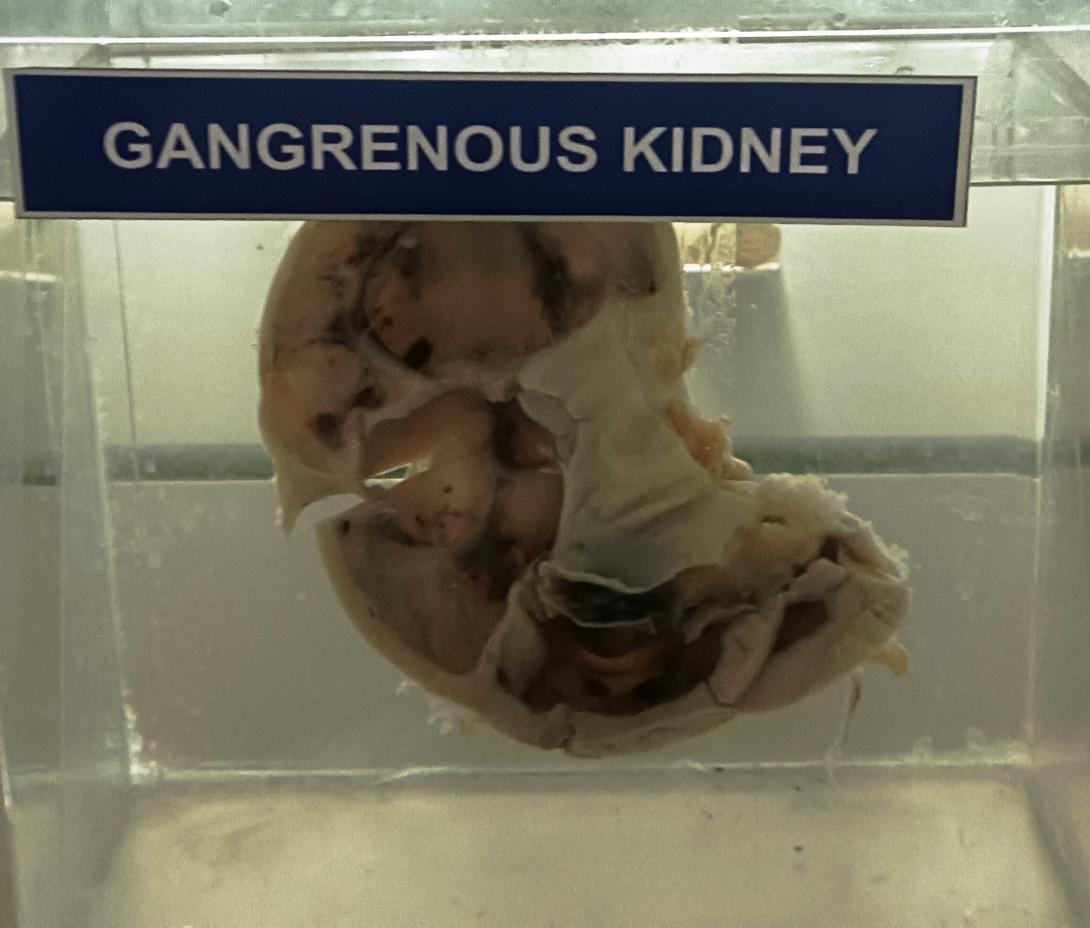
The pathology of gangrenous kidney involves the progressive death of renal tissue due to the lack of oxygen and nutrients that result from the blockage of blood flow. The affected kidney may become swollen and discolored, with areas of necrotic tissue turning black or gray.
As the condition progresses, the kidney may become enlarged and develop abscesses, which can lead to the formation of pus and further tissue damage. In severe cases, the kidney may rupture, causing severe pain and potentially life-threatening complications.
Diagnosis of gangrenous kidney typically involves a combination of medical history, physical examination, and imaging tests such as ultrasound, CT scan, or MRI. Treatment may include medications to dissolve blood clots, surgery to remove the affected tissue, or, in some cases, removal of the entire affected kidney.
In some cases, gangrenous kidney may be asymptomatic or cause only mild symptoms, making early detection and treatment critical for preventing further tissue damage and preserving kidney function.