Placental circulation[edit]
Maternal blood fills the intervillous space, nutrients, water, and gases are actively and passively exchanged, then deoxygenated blood is displaced by the next maternal pulse.
Maternal placental circulation[edit]
In preparation for implantation of the blastocyst, the endometrium undergoes decidualization. Spiral arteries in the decidua are remodeled so that they become less convoluted and their diameter is increased. The increased diameter and straighter flow path both act to increase maternal blood flow to the placenta. There is relatively high pressure as the maternal blood fills intervillous space through these spiral arteries which bathe the fetal villi in blood, allowing an exchange of gases to take place. In humans and other hemochorial placentals, the maternal blood comes into direct contact with the fetal chorion, though no fluid is exchanged. As the pressure decreases between pulses, the deoxygenated blood flows back through the endometrial veins.
Maternal blood flow begins between days 5–12,[19] and is approximately 600–700 ml/min at term.
Fetoplacental circulation[edit]
Further information: Fetal circulation
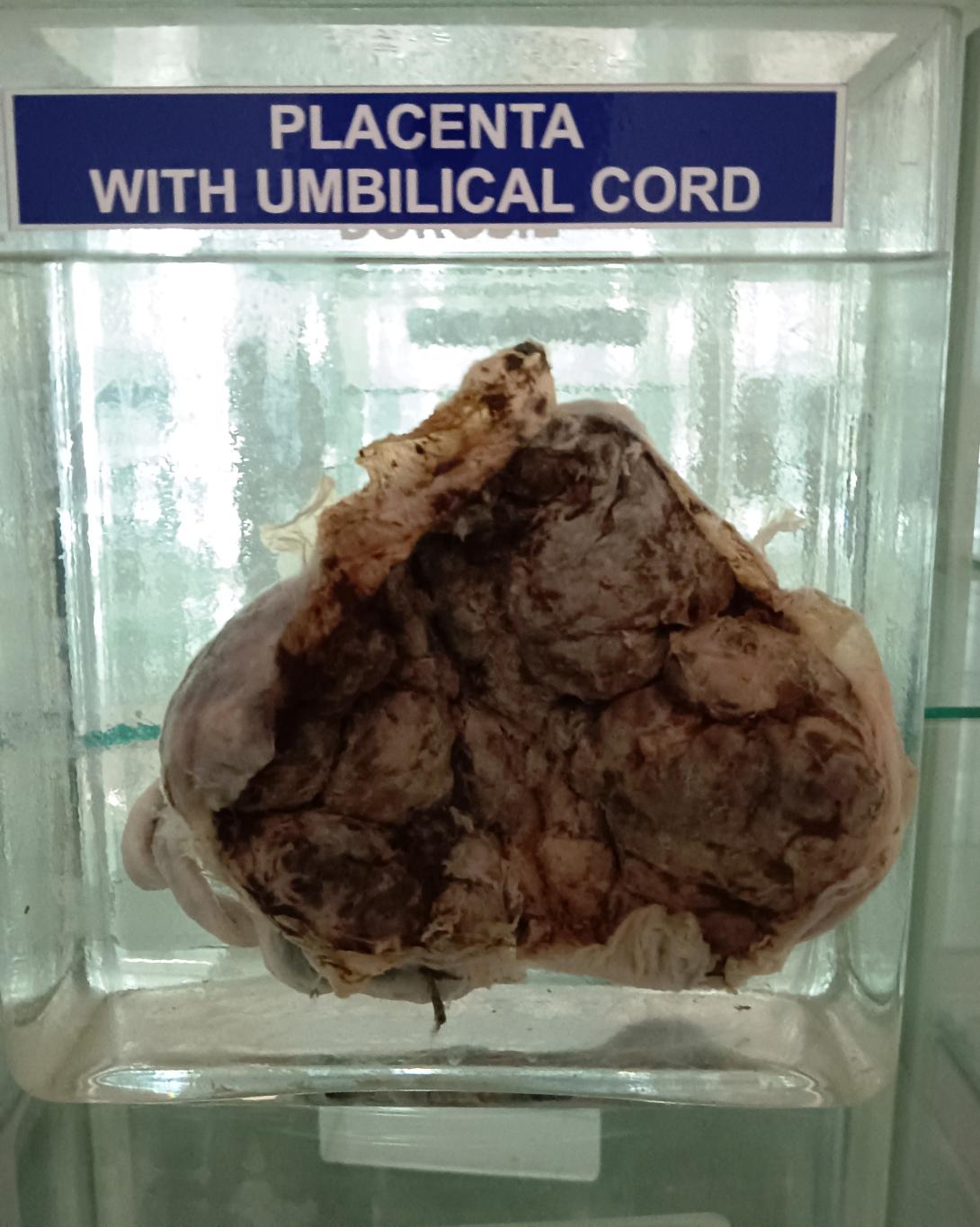
Deoxygenated fetal blood passes through umbilical arteries to the placenta. At the junction of umbilical cord and placenta, the umbilical arteries branch radially to form chorionic arteries. Chorionic arteries, in turn, branch into cotyledon arteries. In the villi, these vessels eventually branch to form an extensive arterio-capillary-venous system, bringing the fetal blood extremely close to the maternal blood; but no intermingling of fetal and maternal blood occurs ("placental barrier").[20]
Endothelin and prostanoids cause vasoconstriction in placental arteries, while nitric oxide causes vasodilation.[21] On the other hand, there is no neural vascular regulation, and catecholamines have only little effect.[21]
The fetoplacental circulation is vulnerable to persistent hypoxia or intermittent hypoxia and reoxygenation, which can lead to generation of excessive free radicals. This may contribute to pre-eclampsia and other pregnancy complications.[22] It is proposed that melatonin plays a role as an antioxidant in the placenta.[22]
This begins at day 17–22.[23]
Birth[edit]
Main article: Placental expulsion
Placental expulsion begins as a physiological separation from the wall of the uterus. The period from just after the child is born until just after the placenta is expelled is called the "third stage of labor". The placenta is usually expelled within 15–30 minutes of birth.
Placental expulsion can be managed actively, for example by giving oxytocin via intramuscular injection followed by cord traction to assist in delivering the placenta. Alternatively, it can be managed expectantly, allowing the placenta to be expelled without medical assistance. Blood loss and the risk of postpartum bleeding may be reduced in women offered active management of the third stage of labour, however there may be adverse effects and more research is necessary.[24]
The habit is to cut the cord immediately after birth, but it is theorised that there is no medical reason to do this; on the contrary, it is theorised that not cutting the cord helps the baby in its adaptation to extrauterine life, especially in preterm infants.[25]
Microbiome[edit]
Main article: Placental microbiome
The placenta is traditionally thought to be sterile, but recent research suggests that a resident, non-pathogenic, and diverse population of microorganisms may be present in healthy tissue. However, whether these microbes exist or are clinically important is highly controversial and is the subject of active research.[26][27][28][29]
Functions[edit]
Nutrition and gas exchange[edit]
The placenta intermediates the transfer of nutrients between mother and fetus. The perfusion of the intervillous spaces of the placenta with maternal blood allows the transfer of nutrients and oxygen from the mother to the fetus and the transfer of waste products and carbon dioxide back from the fetus to the maternal blood. Nutrient transfer to the fetus can occur via both active and passive transport.[30] Placental nutrient metabolism was found to play a key role in limiting the transfer of some nutrients.[31] Adverse pregnancy situations, such as those involving maternal diabetes or obesity, can increase or decrease levels of nutrient transporters in the placenta potentially resulting in overgrowth or restricted growth of the fetus.[32]
Excretion[edit]
Waste products excreted from the fetus such as urea, uric acid, and creatinine are transferred to the maternal blood by diffusion across the placenta.
Immunity[edit]
The placenta functions as a selective barrier between maternal and fetal cells, preventing maternal blood, proteins and microbes (including bacteria and most viruses) from crossing the maternal-fetal barrier.[33] Deterioration in placental functioning, referred to as placental insufficiency, may be related to mother-to-child transmission of some infectious diseases.[34] A very small number of viruses including rubella virus, Zika virus and cytomegalovirus (CMV) can travel across the placental barrier, generally taking advantage of conditions at certain gestational periods as the placenta develops. CMV and Zika travel from the maternal bloodstream via placental cells to the fetal bloodstream.[33][35][36][37]
Beginning as early as 13 weeks of gestation, and increasing linearly, with the largest transfer occurring in the third trimester, IgG antibodies can pass through the human placenta, providing protection to the fetus in utero.[38][39] This passive immunity lingers for several months after birth, providing the newborn with a carbon copy of the mother's long-term humoral immunity to see the infant through the crucial first months of extrauterine life. IgM antibodies, because of their larger size, cannot cross the placenta,[40] one reason why infections acquired during pregnancy can be particularly hazardous for the fetus.[41]
Endocrine function[edit]
- The first hormone released by the placenta is called the human chorionic gonadotropin (hCG) hormone. This is responsible for stopping the process at the end of menses when the corpus luteum ceases activity and atrophies. If hCG did not interrupt this process, it would lead to spontaneous abortion of the fetus. The corpus luteum also produces and releases progesterone and estrogen, and hCG stimulates it to increase the amount that it releases. hCG is the indicator of pregnancy that pregnancy tests look for. These tests will work when menses has not occurred or after implantation has happened on days seven to ten. hCG may also have an anti-antibody effect, protecting it from being rejected by the mother's body. hCG also assists the male fetus by stimulating the testes to produce testosterone, which is the hormone needed to allow the sex organs of the male to grow.
- Progesterone helps the embryo implant by assisting passage through the fallopian tubes. It also affects the fallopian tubes and the uterus by stimulating an increase in secretions necessary for fetal nutrition. Progesterone, like hCG, is necessary to prevent spontaneous abortion because it prevents contractions of the uterus and is necessary for implantation.
- Estrogen is a crucial hormone in the process of proliferation. This involves the enlargement of the breasts and uterus, allowing for growth of the fetus and production of milk. Estrogen is also responsible for increased blood supply towards the end of pregnancy through vasodilation. The levels of estrogen during pregnancy can increase so that they are thirty times what a non-pregnant woman mid-cycles estrogen level would be.
- Human placental lactogen (hPL) is a hormone used in pregnancy to develop fetal metabolism and general growth and development. Human placental lactogen works with growth hormone to stimulate Insulin-like growth factor production and regulating intermediary metabolism. In the fetus, hPL acts on lactogenic receptors to modulate embryonic development, metabolism and stimulate production of IGF, insulin, surfactant and adrenocortical hormones. hPL values increase with multiple pregnancies, intact molar pregnancy, diabetes and Rh incompatibility. They are decreased with toxemia, choriocarcinoma, and Placental insufficiency.[42][43]
Immunological barrier[edit]
Further information: Immune tolerance in pregnancy
The placenta and fetus may be regarded as a foreign body inside the mother and must be protected from the normal immune response of the mother that would cause it to be rejected. The placenta and fetus are thus treated as sites of immune privilege, with immune tolerance.
For this purpose, the placenta uses several mechanisms :
- It secretes neurokinin B-containing phosphocholine molecules. This is the same mechanism used by parasitic nematodes to avoid detection by the immune system of their host.[44]
- There is presence of small lymphocytic suppressor cells in the fetus that inhibit maternal cytotoxic T cells by inhibiting the response to interleukin 2.[45]
However, the placental barrier is not the sole means of evading the immune system, as foreign fetal cells also persist in the maternal circulation, on the other side of the placental barrier.[46]