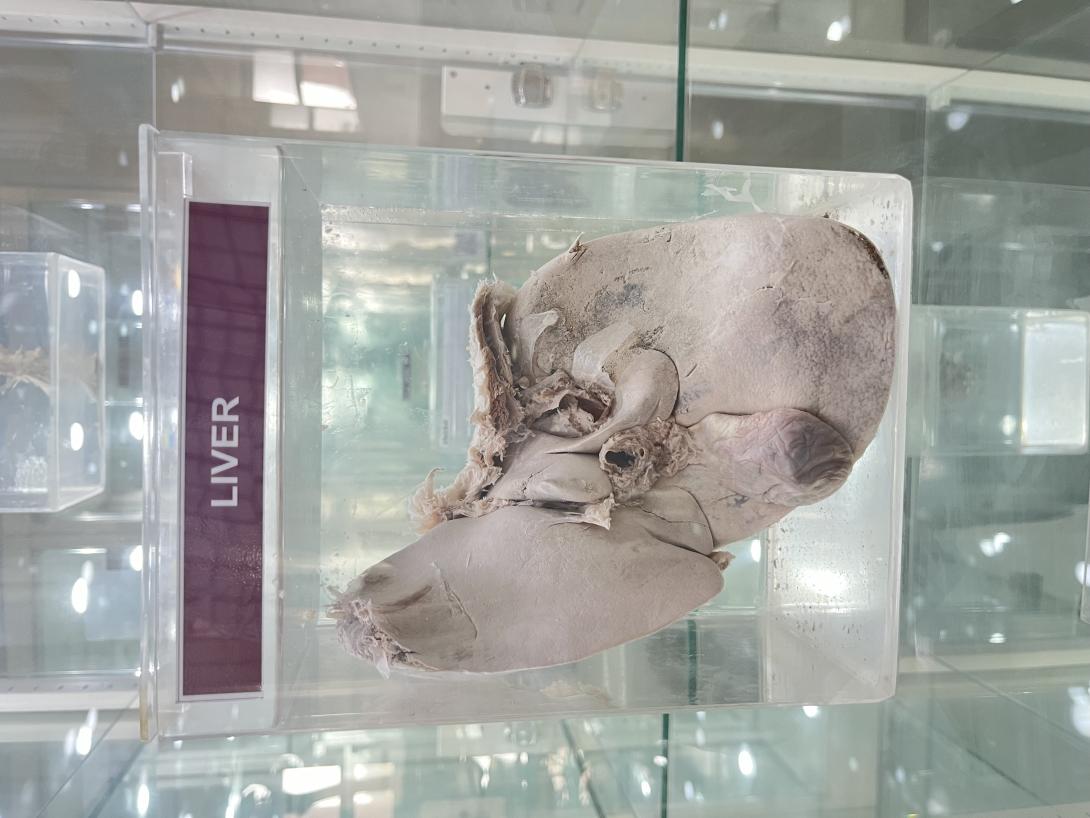
Clinical Relevance: Percutaneous Liver Biopsy
A percutaneous liver biopsy is procedure used to obtain a sample of liver tissue. A needle is inserted through the skin to access the liver.
The biopsy is required in several clinical scenarios:
- Abnormal LFTs of unknown cause.
- Liver malignancy
- Hepatitis C – Assessment for severity of liver fibrosis and disease progression.
- Other liver conditions (such as Hereditary Haemochromatosis and Autoimmune Hepatitis).
- Following liver transplantation.
During the procedure, the liver is located via ultrasound from a subcostal approach (under the ribs). Local and deep anaesthetic is injected where good liver tissue can be seen and the needle path is free of vessels. The patient is asked to hold their breath and the biopsy is obtained.
If a patient has abnormal clotting (a relative contraindication), a percutaneous biopsy while platelets are running, or a transvenous liver biopsy can be attempted. This involves cannulating the internal jugular vein, and passing the biopsy needle through to the hepatic veins, allowing for a biopsy sample to be taken.
Malignant lesions of the liver represent metastasis from other primary cancers in 90% of cases, with primary liver malignancies being relatively rare. Of the primary liver cancers, 90% are hepatocellular carcinoma (HCC), with intrahepatic cholangiocarcinoma making up the remainder.
Hepatocellular carcinoma is the sixth most common cancer worldwide and the second leading cause of cancer death. Incidence rates vary significantly across the globe, mainly determined by the incidence of hepatitis B virus (HBV) and hepatitis C virus (HCV) infection; in China there are over 400 cases per 100,000 people, whilst in the UK there are just around 13 cases per 100,000 people.
In the UK, the majority of cases occur in those >70 years old with around 65% of cases occurring in males; in areas of high endemic HBV or HCV infection rates, age of diagnosis is much lower.
Cystic diseases of the liver are relatively common conditions and are most commonly identified incidentally on routine imaging. However, in rare cases they can be complicated and life-threatening.
In this article, we will discuss the varying types of cystic liver disease, their investigation, and management options.
Liver abscesses typically result from a polymicrobial bacterial infection spreading from the biliary or gastrointestinal tract, either via contiguous spread or seeding from the portal and hepatic veins.
Common causes include cholecystitis, cholangitis, diverticulitis, appendicitis, or septicaemia
The most commonly isolated organisms are E. Coli, K. pneumoniae, and S. constellatus, although fungal causes may also be present in immunocompromised patients.